The road to opioid abuse: Prescription drugs
Jump to section…
Tarrant County is thousands of miles away from the epicenter of the nation’s opioid epidemic, but health officials have created a strategy that has helped react to the crisis.
In 2015, a year after deaths from opioid overdoses reached a record high, a coalition of groups that work with drug users began developing a needs assessment, creating a plan of how Tarrant County could help opioid abusers and prevent others from becoming hooked on the deadly drug.
Since then, efforts have included training doctors to look for signs of drug abuse, as well as raising awareness about the dangers inherent with prescribing opioids, educating the public on what signs to look for if they suspect opioid abuse, and sparking a conversation that moves the discussion about drug abuse away from judging opioid users and instead toward understanding and help.
“Tarrant County has always been cutting-edge because of our coalition work on how we’re addressing this issue,” said John
An introduction to opioids
Opioids, which have been around for centuries, mask pain by targeting nerve cell receptors in the body and brain. They come in a variety of forms, including the illegal drug heroin and prescription medicines hydrocodone, morphine, codeine, oxycodone and the synthetic opioid fentanyl.
The most common brands of opioids — OxyContin, Vicodin, Percocet
The effect of opioids in America is staggering:
- The U.S. accounts for 5% of the world’s population, yet consumes 80% of the world’s opioid supply, according to the National Institute on Drug Abuse.
- In 2017, more Americans died of opioid overdoses – 47,600 – than in car accidents, according to the Centers for Disease Control and Prevention.
- More than 2 million Americans have an opioid addiction.
“This is your biggest threat to life,” said Dr. Glenn Hardesty, a local emergency room physician who works with Texas Health and has been fighting on the front lines of the opioid epidemic for over a decade.
While the crack epidemic of the 20th century was particularly hard on some African-American neighborhoods and cities, opioids have struck a
“We’ve had patients as old as 89, and patients as young as 11,” said Matt Zavadsky, the chief strategic integration officer at MedStar Mobile Healthcare, the EMT company that serves the Tarrant County area.
What distinguishes opioid abusers from other addicts is that their drug dependence often began with the use of prescription painkillers, according to the CDC.
Opioid Overdose
The average American has a greater chance of dying of opioid overdose than in a car accident. The drugs suppress one’s respiratory system, and overdoses are identifiable by unconsciousness and losing the ability to breathe.
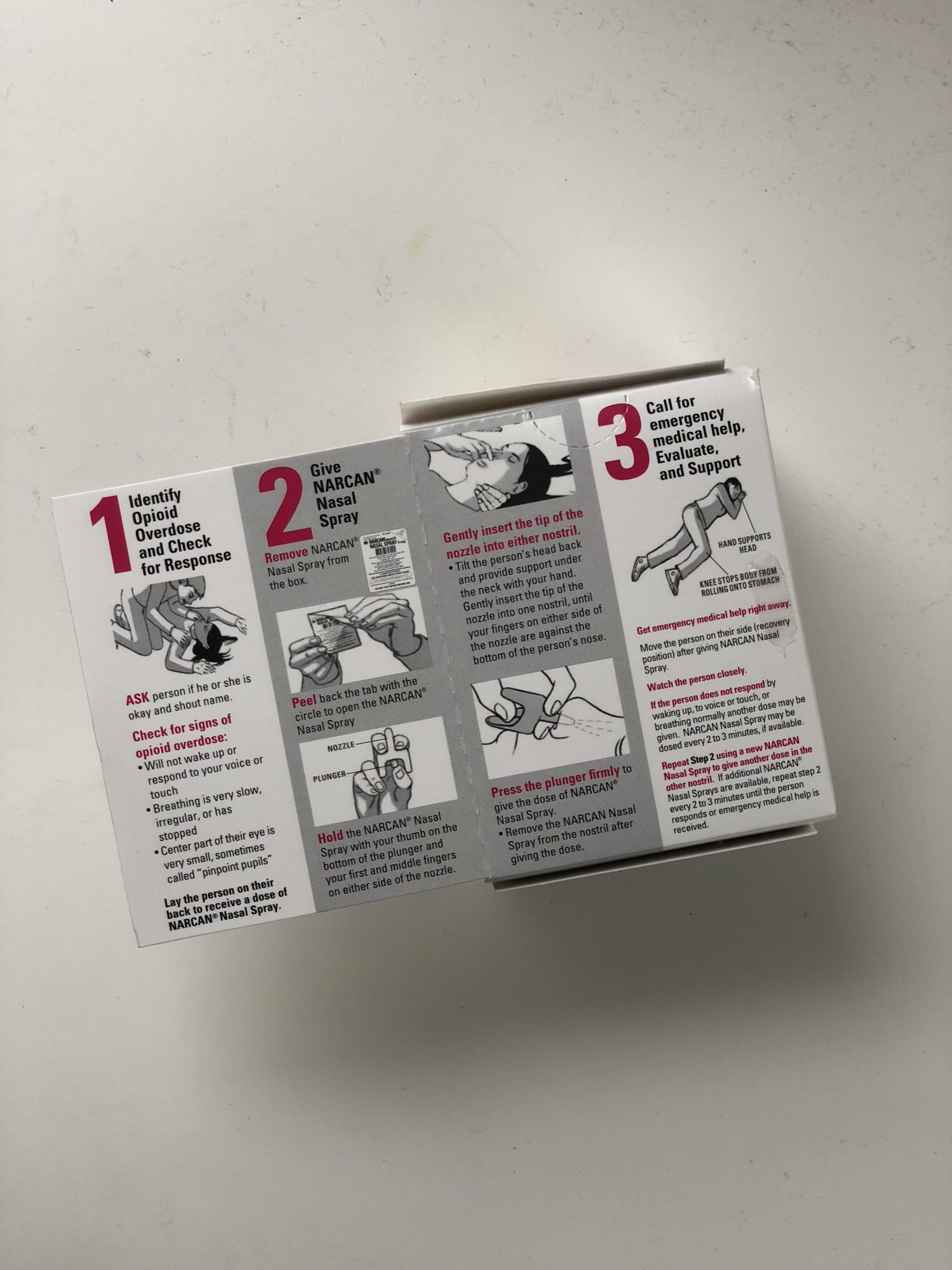
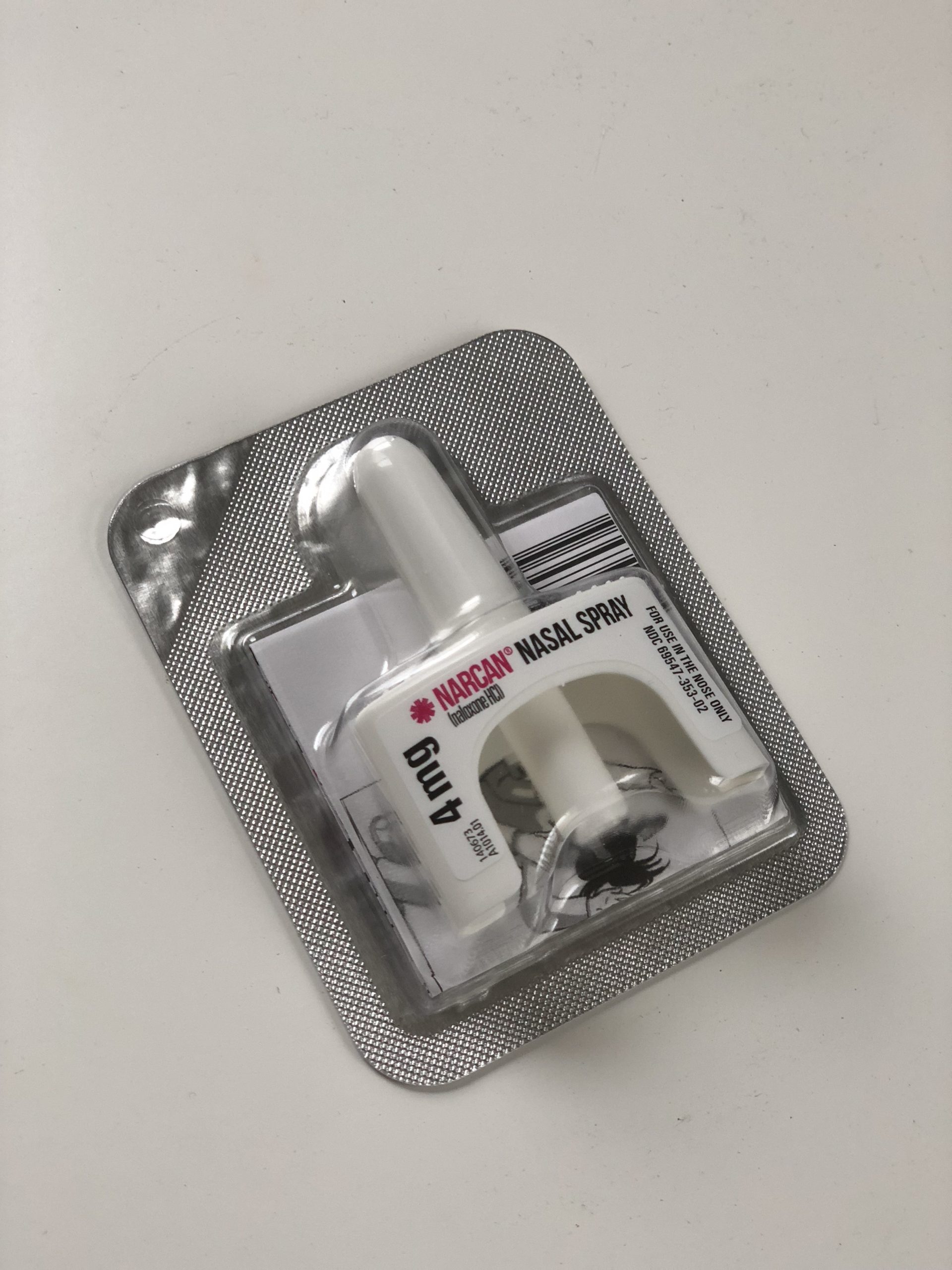
If a user does overdose on opioids to the point of near death, there’s a drug that can instantly reverse the effects of an opioid overdose.
One four-milligram dose of naloxone, better known by its generic retail name Narcan, takes about 30 seconds to save a life. The drug blocks all of the receptors in the body that are susceptible to opioids, so the effect of the opioid is canceled almost immediately. Emergency medics are equipped with the drug, and anyone off the street can buy Narcan in a drug store. Just spray, wait and there you have it: instant overdose reversal.
While the drug itself really is that simple, the aftermath and the societal impact of naloxone accessibility are more complicated.
After counteracting an overdose, the user is thrown out of the high – often resulting in pain, vomiting and anger, Zavadsky said.
Paramedics typically only administer a partial dose: enough to ensure the patient is breathing, but not enough to regain consciousness. Then, the EMTs will take the patient to the hospital for further recovery and to discuss rehabilitation and substance abuse counseling options.
When a civilian administers Narcan and helps the overdosed person regain consciousness, a potentially fatal problem can rise. The user is conscious, breathing, no longer under the effects of the opioids and less likely to seek further medical help.
However, the effects of Narcan only last for around 30 to 45 minutes, whereas opioids can take hours to wear off. By administering the medication at home and refusing transport to the hospital, the user has the potential to slip back into the high and again face dangerous levels of unconsciousness and low breathing.
The availability of Narcan has created an “EMS conundrum.” Increasing the accessibility of Narcan also increases the chances of people overdosing and risking death again, right after the effect wears off.
“Our fear is that we have enabled people to feel safe taking opioids,” Zavadsky said.
Two years ago, while Zavadsky was on an EMS field ride in Baltimore, Maryland, eight of the 11 calls he accompanied were opioid overdoses. All had been given Narcan by family members and friends by the time the paramedics arrived. On one call, a user had overdosed on heroin and his girlfriend had administered the Narcan that saved him.
“So I asked her, ‘Did you get the Narcan from Walgreens?’” Zavadsky said. “She said, ‘No, I got it from his dealer.’
“Of course you did! Of course. If you’re a dealer, you don’t want your customer base to go away. You don’t want them to die. You want them to be able to reverse their overdose so they don’t die so you can keep selling to them.”
Matt Zavadsky, chief strategic integration officer for MedStar.
In 2018, 80% percent of overdose reversals nationwide were carried out by other drug users, according to a report by the CDC.
“You’re between a rock and a hard place because you want to help people, you want to save people,” Zavadsky said. “But are we enabling them to engage in risky behavior?”
If so, that risky behavior is arguably saving lives and giving second chances to opioid users.
“A third of my patients that come in now have received Narcan on the street sometime,” Teater said. “Not in the hospital, but on the street, and they wouldn’t be alive to come in for treatment if that wasn’t available for them.”
O.D. Aid, a local grassroots organization that advocates for opioid harm reduction, advocates for widespread Narcan distribution. Volunteers Lizzie Maldonado, Rachel Gollay and Caitlin Dowdy work with O.D. Aid to distribute “harm reduction supplies,” things like Narcan and condoms that help improve the health and safety of drug users, and to educate the community on “harm reduction principles,” which include information on how to prevent overdoses, how to administer naloxone and the relationship between social stigmas against drug users and criminal policies concerning drug use.
“There’s an assumption that it [Narcan] somehow enables someone to recklessly use drugs, sort of like, ‘Well, I know that I have Narcan on hand so I’m just going to go to town,’” Gollay said. “That’s not the reality. And, I mean, even if it was, arguably, saving a life is the ethical and right thing to do, in my view.”
The stigmas surrounding opioids make people apply judgments to overdose that they do not apply to other poor health choices, said Maldonado, whose green ombré hair matched the colors on her “Real Friends Carry Naloxone” t-shirt.
When someone has a heart attack, no one considers what kinds of foods or how many saturated fats that person ate over his or her life and thinks that information has any impact on whether that individual’s life should be saved, she said.
“No one recovers from death, so how are people supposed to have opportunities to recover and change if they’re dead?” she said. “They can’t.”
Often, a close brush with death by overdose is a teachable moment, Contreras said.
“Sometimes it is very much a wake-up call,” Contreras said. “It may be that first kick to get started and to seek treatment and to look for alternative ways to cope with issues in life, and alternative ways to deal with stress and all of the things that are put on all of our shoulders.”
Sometimes, overdoses alert the relatives and loved ones of drug users of the severity of the problem, and can provide the chance for intervention. Opioid addiction is an easy problem to hide from loved ones, which leads to a greater risk of danger.
Those who are at the highest risk of overdose are users who are potentially using in secret, or are using alone, or do not let others know how much they are using. The stigma and shame around even talking about drug use can prevent users from taking steps to be safe when using, like making sure someone else is home or having a buddy system, Gollay said.
“If you have a loved one who is using an opioid, you should have that medication [naloxone] with you because you do not know what the outcome is going to be,” Haenes said.
“In the face of pain”
From 1999 to 2010, prescription opioid sales nearly quadrupled as physicians began prescribing them to treat chronic pain. Deaths from prescription opioids more than quadrupled, but rather than seeing this as a warning sign, it was initially seen as a weakness in the user.
The surge in prescriptions was being driven by the pharmaceutical industry. One company in particular, Purdue Pharma, which makes OxyContin, reassured physicians and healthcare facilities that opioids were safe treatments for mild to severe chronic pain.
Purdue pushed this drug and other opioids onto physicians and healthcare facilities as safe treatments for mild to severe chronic pain. The company knowingly denied any risks of addiction from opioid use, and other pharmaceutical companies followed their lead.
For years, lobbyists of pharmaceutical companies worked the halls of Congress to block legislative restrictions and regulations on prescription opioids. The Centers for Medicare & Medicaid Services tied hospital and physician payments to patient satisfaction scores. One section on these patient satisfaction surveys asked about pain management and pain medication provision, which provided another incentive for healthcare providers to prescribe opioids.
These restrictions were replaced in 2018 with questions on “communication about pain,” and in July 2018, the CMS proposed to throw out these questions altogether, following the
Dr. Don Teater, a family care physician, recalled a Purdue sales representative telling him to start prescriptions with a 10 mg dose of OxyContin twice a day for chronic pain patients, and to have the patients come back weekly.
He said the sales representative suggested doubling the dose until the pain stopped and assured him a patient who truly had pain wouldn’t get addicted. In reality, the CDC warns the higher the dose, the higher the risk of overdose and death.
Dr. Don Teater
“I know several of my patients who died because of my opioid prescribing and it was clearly my trust in Purdue Pharma and their representatives that led me, and all the other physicians, down that road.”
Last month, New York became the latest state to sue Purdue Pharma over the deceptive practices that increased the opioid dosage and prescription rates, which in turn increased overdose and death rates.
Internal documents and communications from Purdue were included in a lawsuit Massachusetts filed against the company. The documents revealed that the company knew about the addictive dangers of the drug, the relationship between increased dosage and increased risk of overdose, and the profit increase due to increased dosage.
According to the documents, Purdue misrepresented the risk of addiction as virtually non-existent in “trustworthy patients.” There’s also information that suggests Purdue targeted vulnerable populations, including elderly patients and veterans covered by government healthcare like Medicare and Medicaid.
By 2012, the nation was awash in opioid prescriptions. In Tarrant County, prescribers gave out 84.8 opioid prescriptions per 100 people, outpacing the state average of 73.1 prescriptions per 100 people and the national average of 81.3 prescriptions per 100 people.
No more refills
Out of the 91.8 million adults in the United States who used prescription pain relievers in 2015, approximately 11.5 million of them misused them at least once, according to results from the 2015 National Survey on Drug Use and Health.
“Since it’s a prescription, people assume it’s safe,” Haenes said.
The top reason provided by 63.4% of respondents on why they misused their painkillers was “to relieve physical pain.”
Physical pain is not the only reason for self-medication of opioids. According to
“People start chasing that feeling because for the first time in their life they feel normal,” he said. The epidemic took root as some people found themselves still craving the drug after their prescriptions had run out.
“So they’re willing to share, they’re willing to borrow, they’re willing to exceed dosage, and what we know is that it’s absolutely antithetical to everything we’ve been putting out there.”
John Haenes, the Chief Operating Officer of Challenge of Tarrant County,
The alternatives are plentiful and dangerous:
- Illicit prescription painkillers include Xanax or Ativan, classified as benzodiazepines, which are also addictive.
- The Malaysian-imported drug Kratom is unregulated and sold in head shops.
- Large concentrations of loperamide, the active agent in Imodium and other anti-diarrhea drugs, can provide that floaty opium high.
- Roughly 80% of heroin users started with misusing prescription drugs, according to the National Institute on Drug Abuse.
The number of patients treated for opioid overdose in the area has increased by the hundreds over the past few years: from 2015 to 2016, the count jumped from 533 to 824 patients, and then up to 1,062 patients in 2017.
When adjusted to account for population growth, the population percentage that has been treated for opioid overdose has actually started trending down, Zavadsky said. But opioid overdose is still the leading cause of incidental death.
Tarrant County’s opioid overdose death rate was 4.9 per 100,000 people in 2016, which is better than the state average of 10.31 deaths per 100,000 people – and Texas ranks in the bottom five states when it comes to opioid overdose death rates. Nationally, 63,632 people died from opioid overdoses in 2016, according to the CDC.
“Nobody’s ever died from pain. But opioids are the biggest cause of injury-related death in the United States. Pain doesn’t kill you. The treatment for it does.”
Dr. Glenn Hardesty, emergency room physician.
Even though the death rate in Tarrant County is relatively better than that of the state or country, the local rate has still more than doubled since 2010.
The statistics on deaths from opioid-related causes are suspected to not be reported as accurately as they could and, arguably, should be.
Opioid use can have a hand in other causes of death – for example, it can highly increase the risk of unintentional falls in elderly patients, or affect one’s ability to drive unimpaired, leading to motor vehicle accidents. According to Hardesty, the involvement of opioids in these deaths is typically underreported.
Texas doctors are not required to report opioid overdoses like they are deaths from gunshot wounds, he said. Families also often do not want their loved ones’ deaths to be reported as drug overdoses, due to shame and stigma surrounding the issue,
“Despite everything that we’re doing, in the next three or four years that death toll is going to climb,” Haenes said. “Because we’re just not there yet.”
Community efforts
Healing the community from this crisis takes work, not just from improving
Here are some ways to join a coalition. Challenge is affiliated with multiple coalitions in Tarrant County that deal with drug use awareness, including:
- Stay on Track, which aims to increase awareness and knowledge of the risks of substance use in Keller and surrounding communities
- SMART Arlington – Know Your Way, a coalition originally founded on the University of Texas at Arlington campus that works to prevent local youth substance use within the broader Arlington community
- Power 2 Choose, a Texas Christian University organization that works to educate their campus community on making responsible decisions regarding drug use
- S.M.A.R.T. — Smart Mavericks Acting Responsibly Together, UT Arlington’s coalition focused on encouraging healthy behaviors and educating students of drug and alcohol use realities
- Follow Our Lead, Weatherford College’s coalition that works to reduce harmful effects from alcohol, binge drinking
and other drugs - Prevention Provider Coalition, which endeavors to find and provide new substance abuse education and intervention strategies for Tarrant County
- Treatment Provider Coalition, which works to ensure that those seeking substance abuse treatment within Tarrant County can get those services
Along with providing education efforts within the local health care system, Challenge and its affiliated coalitions work to inform parents and families on the realities of the issue, how they can talk to their doctors and how to make better decisions regarding opioid use when it comes to their families.
One of the main points discussed with parents is empowerment through knowledge. If parents know enough about this issue at hand, they can question doctors about things, like if a 30-day supply of painkillers is really a necessary healing component following their child’s wisdom teeth extraction or sports injury, and make decisions to get their opioid prescriptions only partially filled.
Patients are not limited to just affecting prevention by making better prescription decisions. They can also talk to their doctors about medication-assisted treatments. By asking if their doctors are licensed or can become licensed Suboxone providers, these patients are helping other individuals –potentially themselves and their family members, too – recover from opioid use disorder in the future, Teater said.
“Doctors will listen to their patients,” Teater said. Unless there’s a little more push for doctors to get certified and actually prescribe medication-assisted treatments, not much is going to change, he said. By having these conversations with doctors, patients can impact their community on both sides of the issue.

(AP Photo/Patrick Semansky)
“When you’re empowered, you’re able to make much better decisions,” Haenes said.
Challenge and different local coalitions also help empower parents and families to have conversations about drug use amongst themselves, even if those conversations can sometimes be uncomfortable.
It might sound ridiculous that while we witness drug use daily in television shows, song lyrics, movies, video games
“It’s not because that parent is choosing to be negligent,” Haenes said. “It’s because they’re in shock and there’s such shame attached to it. They don’t really want to talk about it outside of the family. They don’t know where to go for help. They don’t know what to do, so they’re fumbling their way through it.”
There are resources within the local school systems and the community that can help answer “what do I do now?” and how to prevent it in the first place. Prevention efforts start with early conversations and not waiting until there is a problem to discuss issues like drug use, smart decision making and the day-to-day details of everyone in the family’s lives.
Changing prescription habits

Haenes, with Challenge Tarrant County, said medical schools typically spend eight to 12 hours of instruction on pain, opioids and opioid addiction. This can result in the development of prescribing habits that enable unhealthy use and abuse of opioids.
“Unfortunately, for many doctors, once they leave medical school, getting continuing medical education is a challenge and what they receive in medical school on pain, opioids and addiction is limited.”
John Haenes, the Chief Operating Officer of Challenge of Tarrant County
One of Challenge’s initiatives is to provide continuing education to physicians and other healthcare prescribers.
Mary Ann Contreras, the violence and injury prevention manager for Trauma Services at JPS Health Network, frequently partners with Challenge through community coalitions, and also spearheads opioid education within the JPS Health Network, specifically concerning opioid prescription habits regarding trauma patients.
Over the past three years, Teater has spoken at approximately 50 workshops with local physicians about new research on why opioids are not a reliable, long-term solution to pain.
He has also suggested pain treatment alternatives, including a combination of ibuprofen and acetaminophen, which were shown in blind studies to reduce pain much more efficiently than opioids.
Opioids are suggested only for patients who are suffering from acute pain, like severe burns or major injuries, who can benefit from receiving opioids quickly after their injury, Teater said.
Terminally ill, palliative care, and oncology patients that are struggling with immense pain can also benefit from the pain-reducing qualities of opioids, Hardesty said.
The workshops have been effective.
“Our physicians were blown away,” Contreras said.
They created a Physician Task Force, which implemented new programs to electronically look at the way they prescribe in the JPS Health System. When a doctor places an order for an opioid on their electronic health records, a text box appears providing information on the patients’ opioid prescription history, and suggests other methods of pain relief or a shorter prescription time.
There’s also an effort to remind people that experiencing pain following an injury or procedure is normal. The process of pain management should be targeting how to reduce that pain to an acceptable, reasonable amount, Hardesty said.
Beginning Sept. 1, 2019, pharmacists and prescribers will be required to check an electronic database, called the Texas Prescription Monitoring Program, to see a patient’s prescription history before prescribing or dispensing medications. The program is intended to help prevent cases of duplicate prescriptions and bring attention to other cases of inappropriate use or overprescribing.
The lack of treatment options
“We know that one out of 10 people that need addiction treatment actually receive it,”
Limited resources make addressing the epidemic far more difficult, he said.
People with insurance or money can typically get treated for
But waiting lists are long for those without financial resources or insurance.
“It’s disheartening for that patient because they want to get treatment,” Contreras said.
“That, unfortunately, is a driving factor: you have to give people hope,”
My Health, My Resources, the county-sponsored addiction and mental health service program, is working to deliver some alternative options to lack of funding for spots in residential substance abuse treatment facilities.
One in three patients who enter the MHMR program is admitted for opioid-related substance abuse. It offers outpatient detox and recovery programs.
Users who want to recover, but cannot afford or get a residential treatment spot, can go into to the MHMR office and begin to address the issue by talking to doctors and nurses, getting their vitals taken, being prescribed medication-assisted treatments and more.
One of these medication-assisted treatments is the prescription of Suboxone, which is the generic brand of the drug buprenorphine.
It relieves pain, provides a way for users to be weaned off their addictions, and lessens withdrawal symptoms by providing diminished opioid doses in conjunction with blocking the opioid receptors, according to information from American Addiction Centers.

The use of Suboxone has proven to help with opioid addiction and death rates. When France saw an increase in opioid overdose deaths in the 1990s, it started prescribing Suboxone and reduced the opioid death rate by almost 80% in four years.
The U.S. has strict restrictions when prescribing Suboxone: doctors have to become a licensed approval source by taking an eight-hour course and subsequently passing a test on the material. Then, they can only treat 30 patients with medication-assisted treatments in their first year following their certification and only 100 patients in following years, according to the National Alliance of Advocates for Buprenorphine Treatment.
There is also a lack of doctors that are interested in getting licensed for medication-assisted treatments.
Sometimes it is due to the stigma surrounding treatment of drug users, or due to an unwillingness to participate in the extra training and monitoring of their prescription habits, or just ignorance of the scope of the situation,
Getting opioids out of the community

Along with educating the community on different risks and prevention methods, perhaps the most significant way to help combat this problem is to get opioids out of the community.
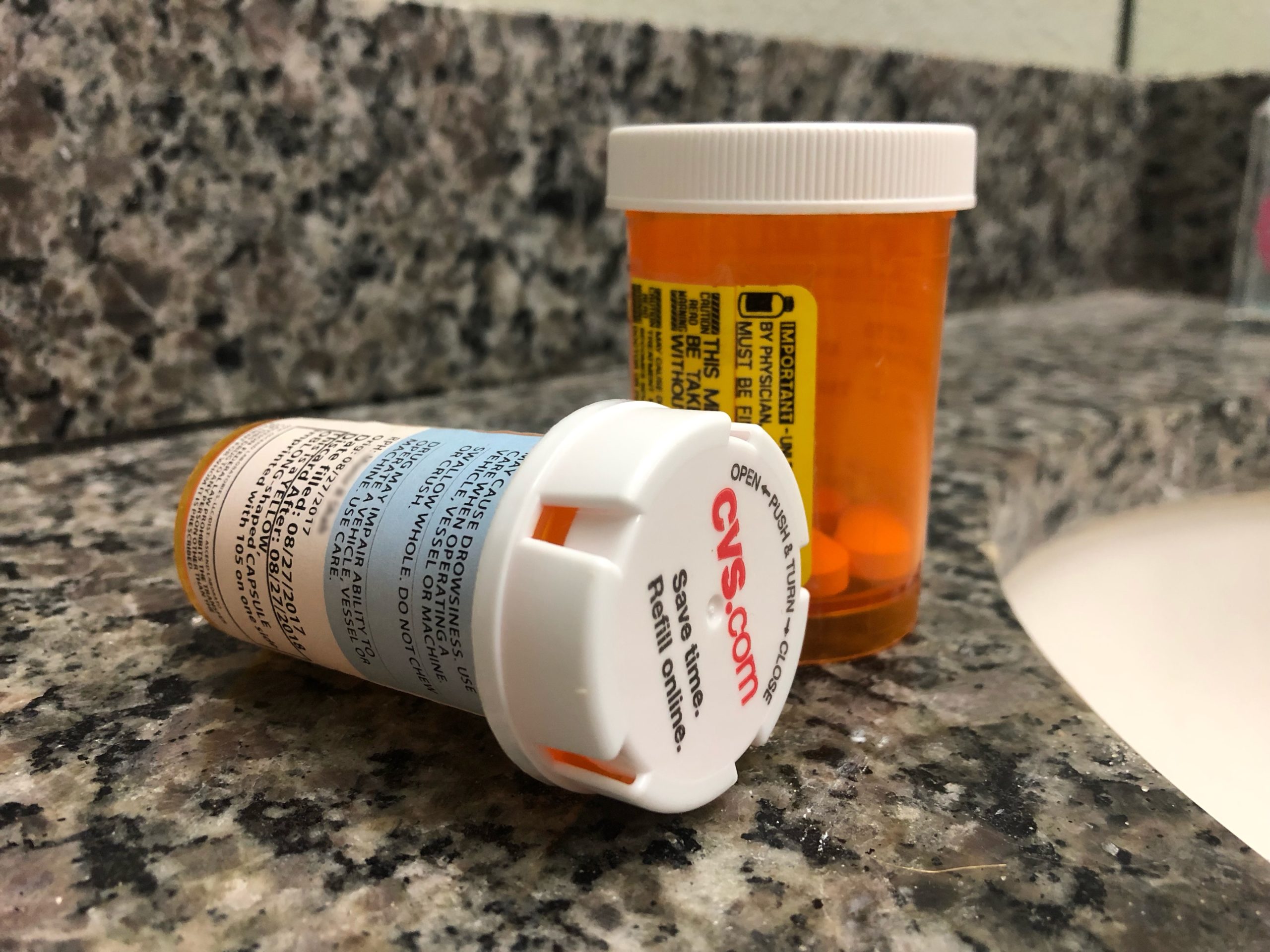
Old drugs that are leftover from past prescriptions and tucked away in medicine cabinets are one of the first places abusers look to easily access opioids.
Improper disposal of prescription drugs, like flushing them down the toilet or just tossing them out in the trash, contaminates the environment, which is not the best method of preventing harm from opioids in the community. The good news is that it is relatively easy to get your old painkillers safely destroyed.
One option is a new innovation – drug deactivation pouches. They’re made by a company called
The Drug Enforcement Agency holds a National Prescription Drug Take Back Day twice a year in spring and fall, where citizens are encouraged to come and dispose of their old prescriptions. The next National Prescription Drug Take Back Day is Saturday, April 27.
There are also prescription drop-off boxes available for use throughout the year. There are 24 drop-off boxes in Tarrant County, located at different pharmacies and police and sheriff offices. They look like giant versions of the mail drop-off boxes at post offices and work just as easily: people drop in their pill bottles, and the drugs get safely incinerated.